If you really felt you were at risk of a heart attack, and you knew that your lifestyle was part of the risk, would you change your lifestyle?
I know I would.
Sadly, one of the issues with the “a pill for an ill” model, where someone else takes responsibility for your health and you abdicate, is it tends to take away the fear.
You focus on one marker of your health and put all your eggs into that one basket.
In this case cholesterol.
High cholesterol = high risk for CVD, therefore low cholesterol = lower risk.
Therefore, why bother changing the food you eat, the amount you move, the way you live your life?
Your cholesterol is now low, so is your risk, so you carry on.
In fact, you might even feel like you are protected and that lifestyle matters even less.
This is exactly what researchers have found in a recent long term study of patients taking statins vs those that do not.
Over the period of ten years after prescription, they slowly increase their calories, up by 14%.
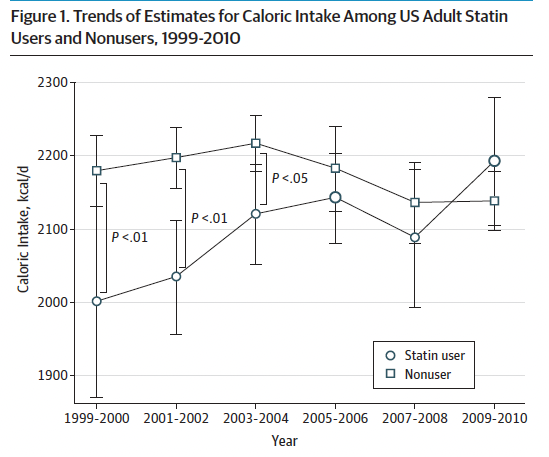
They conclude:
“One possibility is that statin use may have undermined the perceived need to follow dietary recommendations.
Patients who recognized that their LDL-C levels were lowered drastically by statins may have lost the incentive to pursue dietary modifications.
Physicians might have contributed to this process by
shifting the focus of consultations from diet to statin regimen adherence once statin treatment had begun. This hypothesis is compatible with the lower cholesterol levels seen among statin users than among nonusers in later survey cycles”.
I have seen this time and time again, especially with diabetes type 2.
This is without a doubt the clearest example of the medical system actively encouraging dependency.
For the vast, VAST majority of diabetes patients, diet is the cause of their insulin insensitivity.
We can argue about statins and if cholesterol is actually the cause the heart attacks, I would argue against it in most cases.
And point you towards the idea that statins are a mild anti-inflammatory as we discussed previously.
And by bringing inflammation down, they reduce the risk of CVD, albeit very modestly.
Re-read ????

But 99%, your diet causes your diabetes.
But, because we can control the blood sugar with the drug metformin, you can leave the root cause in place 100% and carry on regardless.
This, in my opinion, is unethical.
They are controlled diabetics, still with far higher risks of CVD and many other issues.
We know what works, we talked about it here:
Check it ????

Especially the low carb diet:
https://nutrition.bmj.com/content/early/2023/01/02/bmjnph-2022-000544.abstract?lid=317
They average weight loss of 10kg – let that one sink in !!
No counting calories, no bulls**t weekly weigh-ins with slimming world telling you about food “sins“, just eat real/whole food with an emphasis on higher fat and protein and low(er) carbohydrate.
HbA1c (glycoslyated haemoglobin – a long term marker of blood sugar control, is effectively how sticky your haemoglobin is) dropped from 63 to 46 mmol/mol (note under 42 is normal, 42-48 pre-diabetic and over 48 diabetes).
Blood cholesterol levels fell on average by 0.5 mmol/L and triglycerides by 0.9 mmol/L – It is worth remembering that an LCD is also a high fat diet.
It is often the over consumption of highly processed carbohydrates which leads to an excess of sugar in the blood that must then be turned into fat that can lead to the elevation of cholesterol and triglycerides.
The overall remission rate was 51%, with that figure rising to 77% for those diagnosed within the last year.
Again, let that sink in – half of all T2D patients that agreed to change their diet in one NHS practice achieved remission.
Even those with a 15 year history had 20% remission rates.
The practice cost of diabetes per patient per year dropped to £4.94 while the national average is £11.30.
Think about that in terms of cost savings for the NHS spending 11.7 billion on diabetes a year.
FYI – if your patients want to reduce their chance of a heart attack, get your metabolic health in order.
You want your fasting glucose, insulin and HbA1c LOW, as there are all very clear risk factors for CVD.
Sugar is inflammatory, inflammation damages you and your arteries. Those need to be repaired and part of that process is packing them with cholesterol.

Plus get HOMOCYSTEINE down:
For that, use METHYL B HERO.

