Last week we started talking about functional blood analysis and the need to always get the patient to request GP notes on your behalf.
Yes, this can be useful for nutrition and improving results from care, but it can also be life saving (and save you a costly insurance claim and a whole lot of guilt).
Two weeks ago, a 77 year old lady came back to see me for the first time in a few years with acute low back pain.
She had open heart surgery in January 2021 for a valve issue and when she was taken in had low haemoglobin, i.e grossly anaemic.
Straight after surgery she was given a blood transfusion and after discharge, her GP did some repeat bloods.
These were declared “normal”.
But as we said last week, what is “normal”?
Within the NHS reference range, plum in the middle? aka optimal in our world.
Within the NHS reference range, right on the edge of low/high?
Out of reference range but “normal” for this patient?
So as ever I asked her to request her results, and sadly for her they were anything but normal.
She was still grossly anaemic at 111 g/L, NHS range is 120-150 g/L, I would ideally like people at 130 g/L minimum, but this varies a lot.
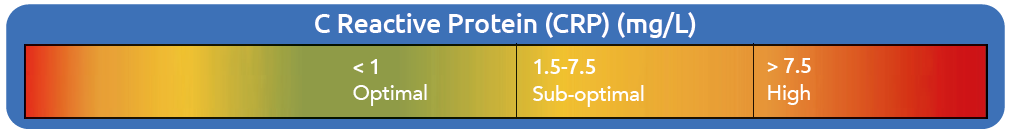
Her C- reactive protein (CRP – a marker of systemic inflammation) was 11 mg/L, normal NHS range is usually 0-7.5 mg/L (though you really want it under 1, certainly under 3).

Now, given she had these done early this year and was still recovering from big surgery, it would not be unreasonable to think they were related and do a follow up with repeat bloods in a few weeks to see if the inflammation and anemia had gone.
Sadly this never happened.
While she has what looks like mechanical low back pain, she is also woefully tired compared to her normal self and terribly stiff and achy, which is all consistent with symptoms of active inflammation and anaemia.
So I sent her back to the GP for repeat tests, while starting some conservative care for her neuro-mechanical issues.
She returned this week, low back feeling better, with new tests in hand.
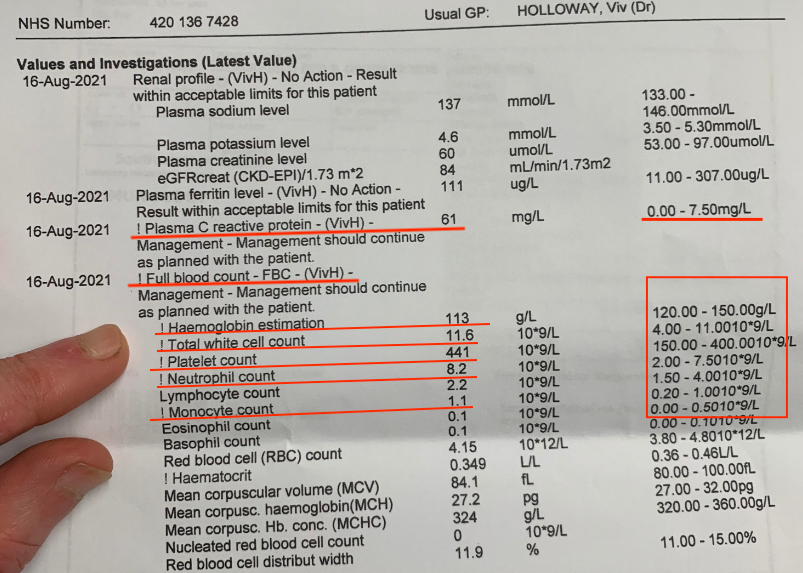
As you can see, the anaemia remains despite 8 months passing since her operation, and we now have significantly raised total white blood cells, and neutrophils and monocytes.
The CRP is now a massive 61 mg/L.
Her ferritin is normal but this doesn’t really help as we do not have a serum iron or iron binding capacity.
Let me explain, ferritin is our long term storage for excess iron.
When we have enough free iron in the blood (serum iron test) to make haemoglobin (and for use in Krebs cycle and for thyroid function), then we stick it into storage (ferritin).
So she is anaemic and one cause could be low iron, but here is the issue of an incomplete iron assessment.
Inflammation is your body’s response to infection, or at least perceived infection. Pathogens need to use the iron for their own metabolism, so the body very cleverly removes iron from the blood to stop the infections getting worse and puts it into storage (ferritin), out of circulation to keep us safe.
Thus, people with long term inflammation from any cause can develop “the anaemia of chronic disease/inflammation”.
You can give them all the iron you want and they will simply remove it from circulation and stay anaemic.
So the issue here is we do not know if she has adequate iron in the blood, and the ferritin is a reflection of that and the anaemia is due to something else.
Or if the iron is being sequestered away from pathogens, resulting in low serum iron and producing anaemia as a consequence.
But the worse part is, with such high white cell counts, we have to consider if she may have multiple myeloma as the cause of their anaemia. This would also explain the massive CRP elevation.
Tthe GP has requested a huge number of tests including bence-jones proteins which are indicative of myeloma. The GP even phoned the patient to give the results. It is amazing what good service you give after you have either mis-read or ignored a blood test and suddenly realise you may have missed a pathology.
So in this case, we were able to hopefully save this patient’s life, and she can get the care she needs, while effectively managing her neuro-mechanical system.
This is what a clinician does.
You look after the patient as a whole and refer out as needed.
You cannot abdicate responsibility for ruling out non-mechanical issues to the medics.
That is what therapists do.
Therapists just treat once the GP has declared “normal” and to hell with the consequences.
It is not good enough.
ACTIONS TO TAKE:
– Never accept “normal”, always get the patient to request the GP blood tests and make your own mind up.
– You can get a full iron panel with serum iron, iron binding capacity, unsaturation and ferritin for only £39 from a finger prick test
https://medichecks.com/
