At some point in your career, if you suggest patients should take any nutritional supplements, eventually you will hear something like this:
“I get all my nutrition from food”
“I don’t take supplements because I eat a balanced diet.”
“Supplements are not absorbed.”
“Supplements give you expensive urine.”
The variations are endless, but the theme is the same.
Now, before we get into the concept of a nutrient gap, that is to say, a gap between what nutrition the patient is getting from their food and what they need to be healthy, and even more importantly, what they need to heal and recover (the latter is going to require a higher intake than for simply maintaining health).
We must point out the elephant in the room.
The vast (vast) majority of your patients have terrible diets, low in nutrients, high in processed foods, sugar, trans fats, refined wheat, alcohol, and prescription drugs.
They have a painful combination of being grossly misled by the media and official guidelines plus being in utter denial they are eating junk food.
Thus, we have an epidemic of below recommended intakes of macro nutrients (protein and keys fats) and micro-nutrients (minerals, water and fat soluble vitamins).
The issue is they have no idea they are deficient, insufficient or suboptimal because the NHS does not test for most these things routinely.
The bits they do check on occasion, like vitamin B12, have such a huge scale/range of “normal”, they routinely miss the symptoms the patient presents with is classic for the nutrient missing – they tend to treat the test, not the patient.
So the patient gets symptoms, goes to the GP, has a test, is told they are all normal and either live the symptoms or takes a drug to mask them.
B12 for example can cause terrible fatigue and low mood (usually in the absence of anaemia), easily misdiagnosed as “depression” and lead to a prescription of SSRI’s often for life.
But let’s pretend they do have a great diet, the question then is, does the food they are eating still have the nutrition today than it did decades ago?
The answer is a very definite no.
The figures vary between studies, between countries and between foods but overall there is a downward trend.
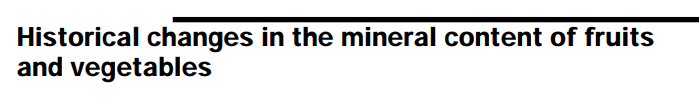
In the UK, one study showed a reduction of 35 % of magnesium in 50 years between the 1930’s to the 1980’s (I would love to know where we are now another 40 years later!)
And in the USA a 6% drop in protein and a 38% drop in vitamin B2, riboflavin.
So yes, whenever you can eat real, whole food, there are many benefits beyond the macro and micronutrients, from fibre to polyphenols.
Try to stick to the rule of high nutrient density with high tolerance to those foods.
This is where eating well cared for animal products can be so important.
The benefits are really in the concentration of nutrition in animals and the forms the come in.
Vitamin A, for example, is found as beta carotene in plants and while that has some key functions, its main job is to be converted to retinol which is the active form of vitamin A, so crucial for immune health and skin.
The conversion can be hugely affected by your genes and nutritional status.
I, for example, hold multiple defects in the gene BCMO that codes to make the enzyme that converts beta carotene to retinol. According to the research means I may convert at 50-60% less than others.
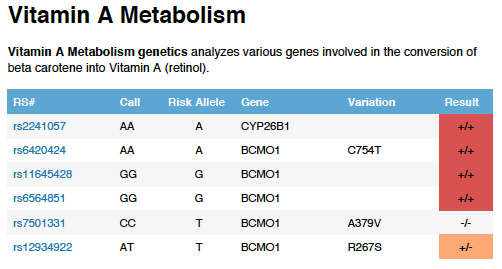
Thus, if I were only to include plant forms of vitamin A, retinol, the active form could slowly, over years, become insufficient, which could affect my immunity and skin health and much more.
In my opinion, this is one of the significant flaws in the argument for a purely plant-based diet.
Note I did not say plant-based, it is entirely possible and often advantageous to have a plant-based diet, but I would always recommend some choice pieces of animal products to give huge bumps in active nutrition as well as plenty of plants.
So, next time patients tell you they are trying to get all their nutrition from food, you can agree they should try, but it is nigh on impossible to do so even with a carefully planned diet.
We call them food supplements because they are a supplement to your food.
From our point of view, low magnesium status may be the difference between clinical success with our care or failure.
Check out this RCT with magnesium supplements for chronic low back pain. Nearly 50% reduction in pain after 6 week, when the magnesium was stopped.
How easy is that?
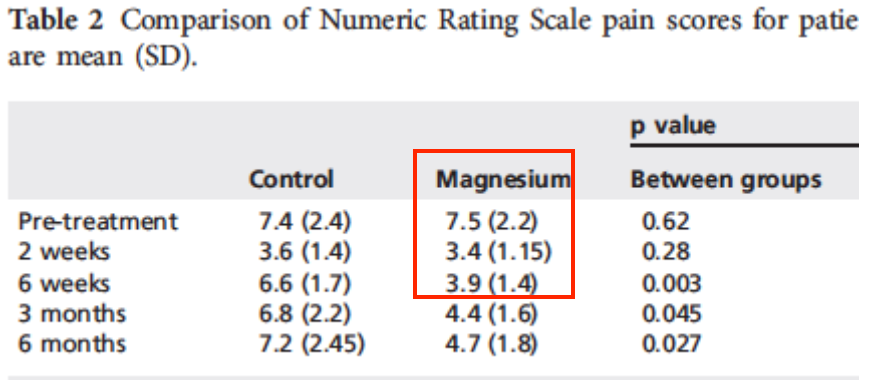
Understanding the nutrient gap, and plugging those gaps with targeted supplements is a quick, easy, cheap and effective way to get your care to work, both significantly and sustainably.
ACTIONS TO TAKE:
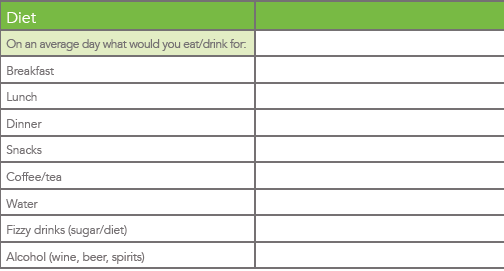
– Always include a little section in your initial intake forms with a section for food intake, never assume what they eat !
Ours looks like this. Bear in mind the “on average” bit can lead to people not being 100% truthful, if in doubt ask for a 3 day diet dairy.
– Keep your eyes peeled over the next few weeks as we move towards the launch of our 3 new products, a comprehensive one a day multi plus two different magnesium products, ideal for plugging gaps and getting results.
