Many years ago, Doctors did not have hundreds of blood tests and scans to rely on, and had to make a diagnosis based on patient history/symptoms, family history and physical examination.
The plethora of tests available today are very, VERY useful, IF, they are integrated into the art of a clinical diagnosis.
That is why we will be launching our blood tests service in Q1 2025.
However, the key part is INTEGRATION of the information from the tests and not a blind faith in the figures they produce.
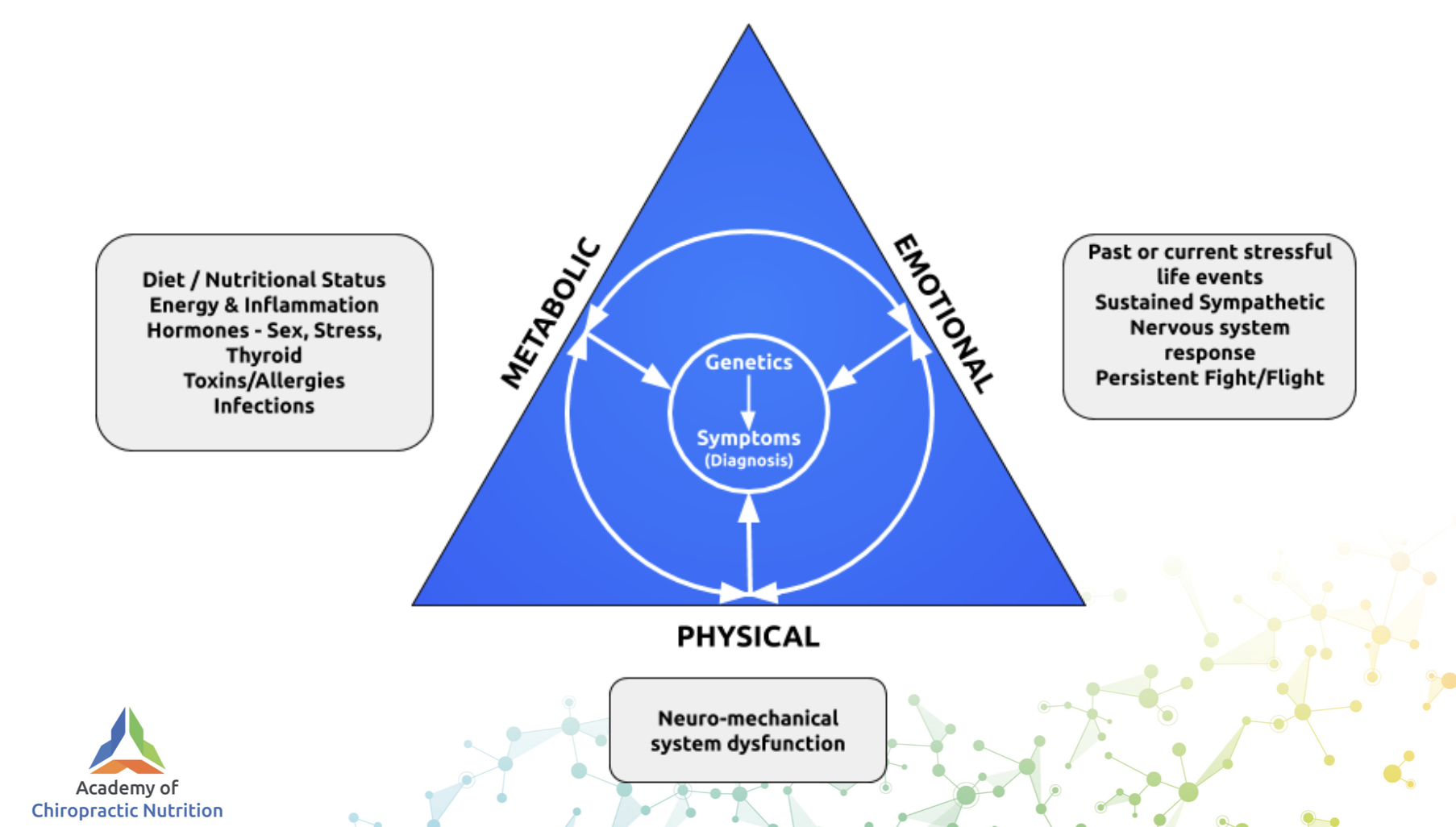
And using a diagnostic lens, that recognises the systems of the body are inter-related.
Hardly a revelation to some, and yet, as we will see, some clinicians have blinkers on that simply stop them seeing reality beyond their immediate view.
All excellent clinicians know this, it is nothing new. But it is in short supply among those who are not dedicated to the path of mastery.
Consider a recent new patient I saw last week, with 11 years of severe left chest pain, diagnosed as “costochondritis”, which can wake him at night.
So bad he has been to A&E multiple times, with many blood tests, MRI’s, ultrasounds and x-rays, all read as “normal”.
He also has pain in his upper left thoracic spine, with occasional pins and needles/numbness into the left arm, less occasionally the right arm.
He is in his mid 30’s, the chest pain is averaging 6-7/10, he uses nortriptyline daily, NSAID’s/co-codamol on and off as needed.
Plus, he is absolutely exhausted.
Also noted on his intake form is a diagnosis of B12 deficiency 6 months ago, he was given injections for a month and then advised to take B12 oral supplements. He takes 1000 mcg in methylcoblamin form.
He eats red meat regularly, and has a history of heartburn/reflux, with loose bowels on and off.
On further questioning, his hands in the morning over the last 3 months are really stiff, he can barely make a fist for the first 2-3 hours.
At this point, I can barely believe that he has not already been diagnosed with inflammatory arthritis, even if it is evolving.
All those scans, the bloods, did they really show nothing?
Or even if they were all negative, surely the clinical picture is screaming, auto-immune disease in process?
Are we really going to wait for enough damage to occur before we give it a name in Latin and make it official?
Well, he sent me his blood tests, so let us take a look at these “normal” tests.
Remember from a previous newsletter, you can have diagnosed inflammatory arthritis, medicated with methoxtrexate and never had a raised inflammatory markers prior to or after your diagnosis.
Below is the CRP of a nine year old boy with very swollen wrists and fingers, subsequently given said drug with a normal CRP.
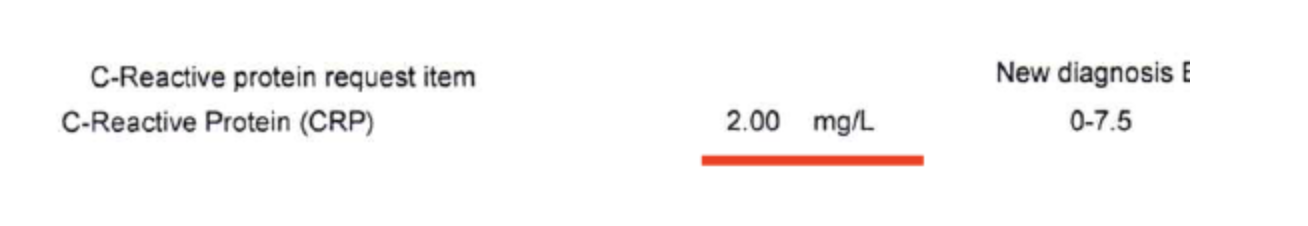
Hence we say:
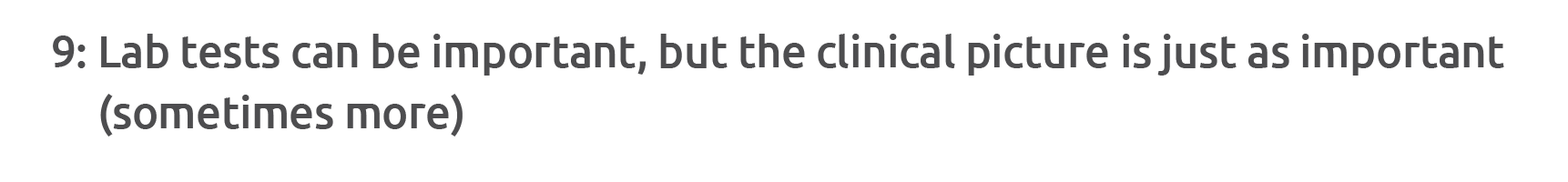
So, let’s take a look at these “normal” results.
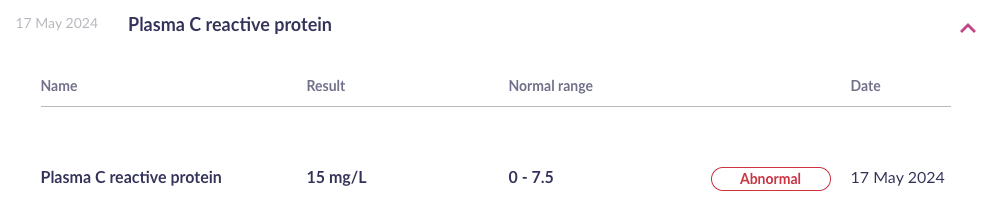
Remember that inflammation is a spectrum, anything over 1 mg/L, is a sliding scale of increasing risk of heart disease, strokes, cancers and all other bad stuff.
????
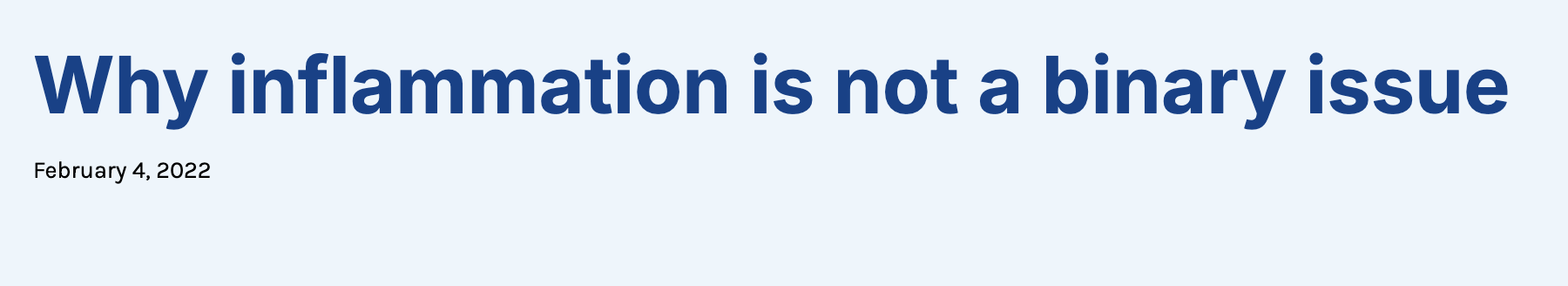
Hence, our FUNCTIONAL range for CRP.
Remember that drug companies 100% know this, hence the stain study known as JUPITER, which says:
“Increased levels of the inflammatory biomarker high-sensitivity C-reactive protein predict cardiovascular events. Since statins lower levels of high-sensitivity C-reactive protein as well as cholesterol, we hypothesized that people with elevated high-sensitivity C-reactive protein levels but without hyperlipidemia might benefit from statin treatment.”
This patient has a very active immune system, his symptoms are textbook, especially hand stiffness in the AM – unless they are >80 year old this is never “normal”.
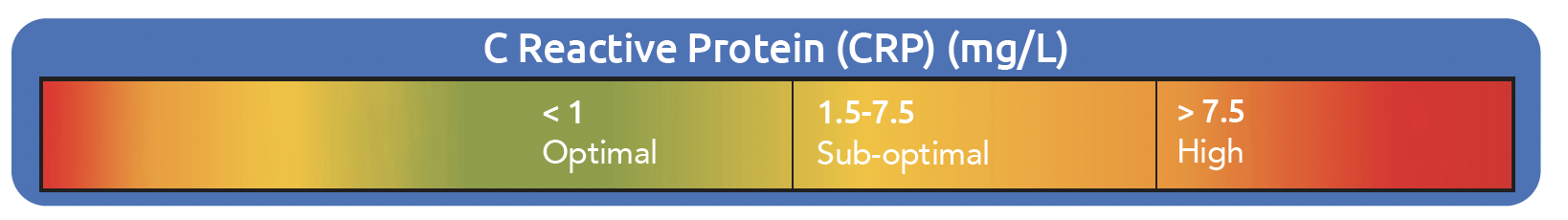
Beyond that, let’s check his vitamin D. Note he is already taking 1000 iu daily, that is 500% of the RDA, must be enough, right?
Oops.
Why would he still be so low?
What are the 3 key risk factors for deficiency?

He is originally from South Africa and his skin tone reflects this and his severe fatigue leaves him unable to exercise and reliant on carbs/sugar.
Thus, he has put on approximately 3 stones in the last few years – vitamin D is a fat, so it is stored in your fat, thus there is less in your blood.
The symptoms of severe/gross deficiency?
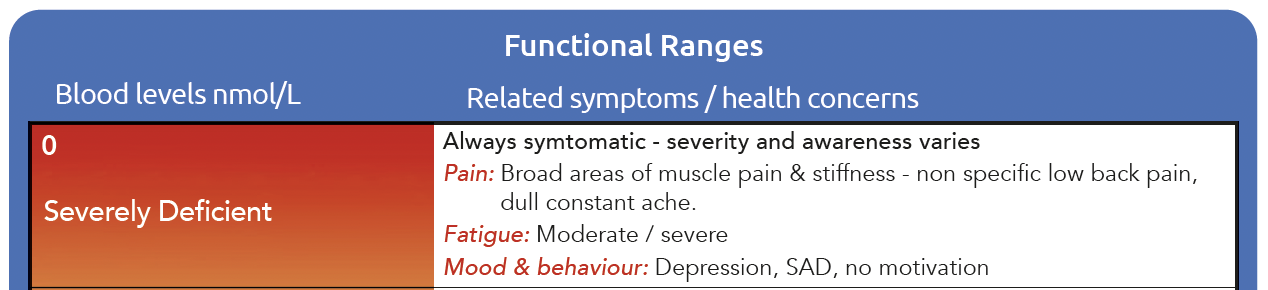
When they are below 25 nmol/L they are ALWAYS tired and in pain.
Could it cause a CRP of 15 mg/L?
That is a bit of a stretch probably, and the pain they get is usually broad and non-specific, and his is quite specific.
But remember, vitamin D deficiency lowers your pain threshold, so could it exaggerate actual physical issues? Yes.
Could you get a physical loss of motion in a rib head from inflammatory damage to the area?
Of course you can.
Damage to the collagen (ligament, bone and cartilage in this case), has to be repaired, and that becomes scar tissue/fibrotic collagen which does not stretch like healthy collagen, hence loss of ROM.
This is why those patients with known inflammatory arthropathy respond well to care, excluding acute flares.
If you want to see how severe the pain from vitamin D deficiency can be check out this case series.
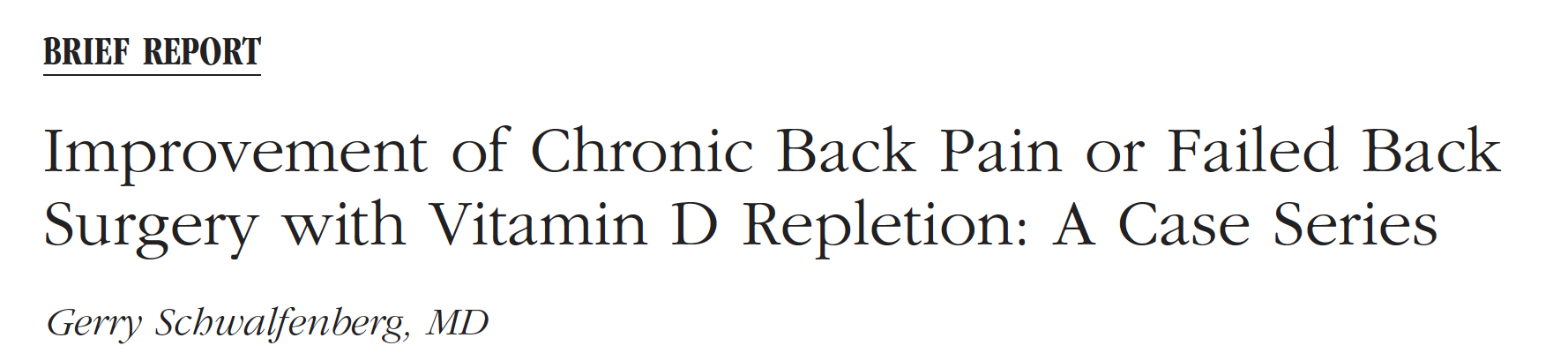
Hope you can read that OK, if not, patient has history of 4 back operations then is diagnosed with “failed back surgery syndrome”. Sees the author and gets diagnosed with 20 nmol/L vitamin D, take 4000 iu daily and has resolution of pain in 6 weeks. ????
But it gets worse, consider his B12 levels.
He was diagnosed B12 deficient but he was eating red meat?
By definition, that means he is not absorbing B12 from food.
If we then give him a swallowed capsule, it is entirely possible that this will also not be absorbed, and he stays low.
Remember his neuro symptoms in not one but both arms?
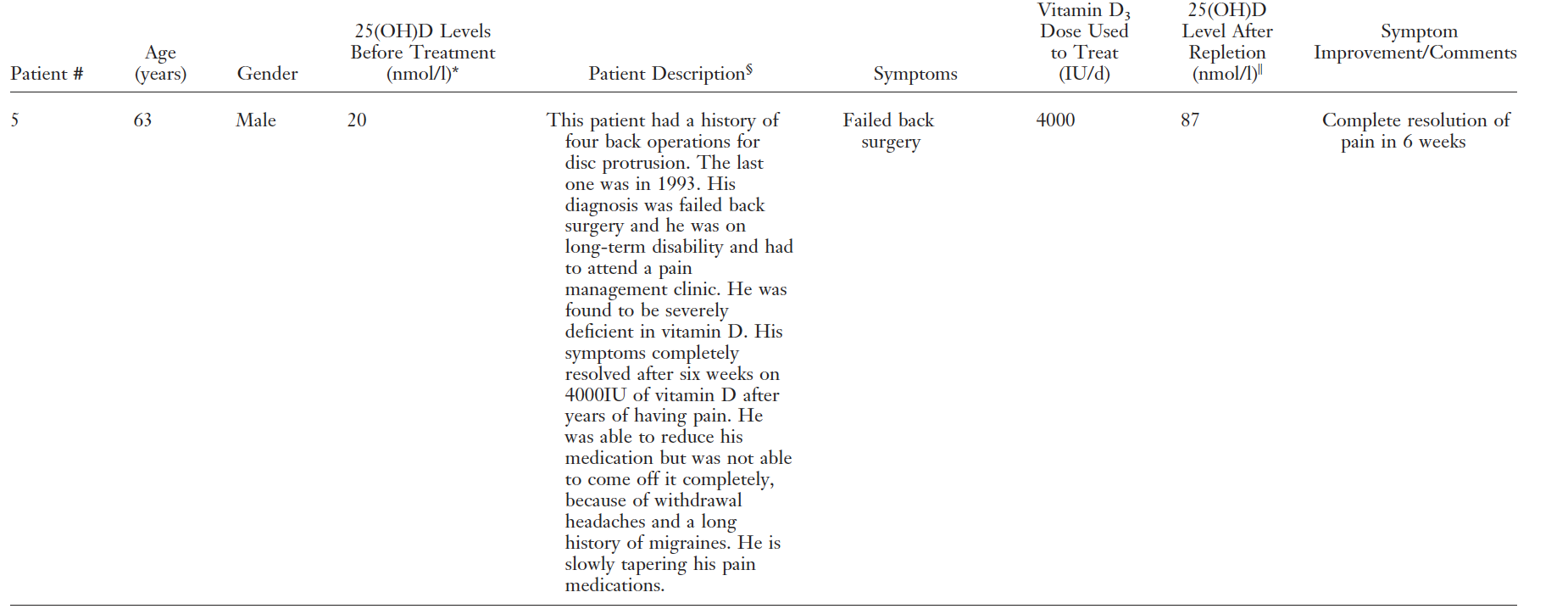
The range for B12, is expressed in two ways, pmol/L and ng/L.
And on top of that, where deficiency begins and ends is a matter of significant debate.
This is our scale:
This is the very recent B12 guidance from NICE.
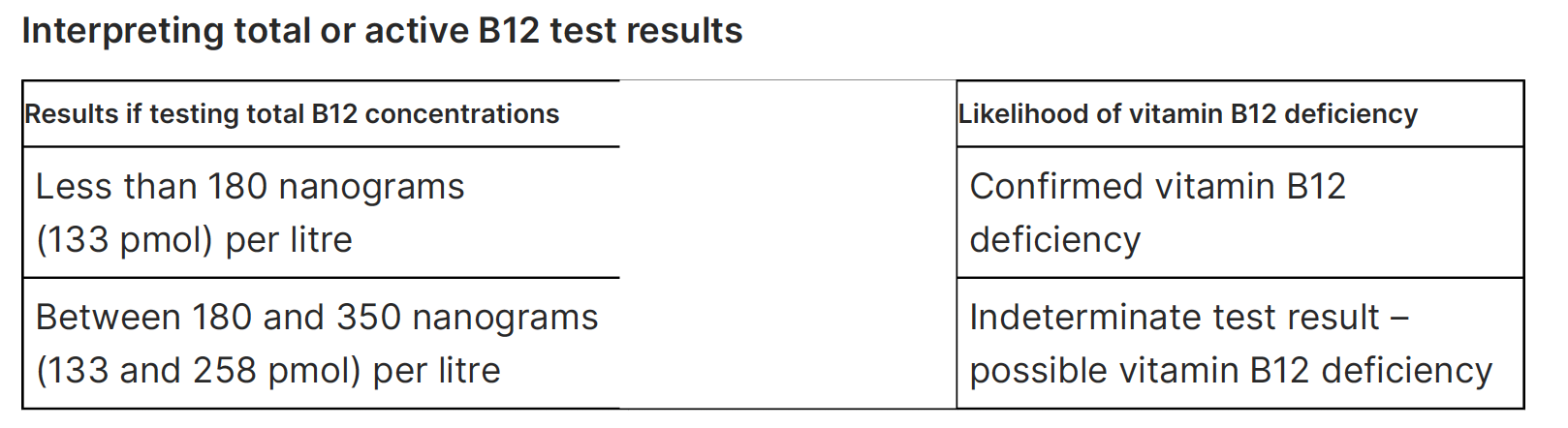
Note they have lowered low cut off point to 133 pmol/L (180 ng/L) but they do now recognise a possible deficiency grey zone up to as high as 258 pmol/L (350 ng/L).
For me, anything under 500 pmol/L(677 ng/L) with symptoms is a green light to trial B12.
His result, 186 ng/L (note they have under 160 ng/L as deficient which is 20 lower than the NICE guidance).
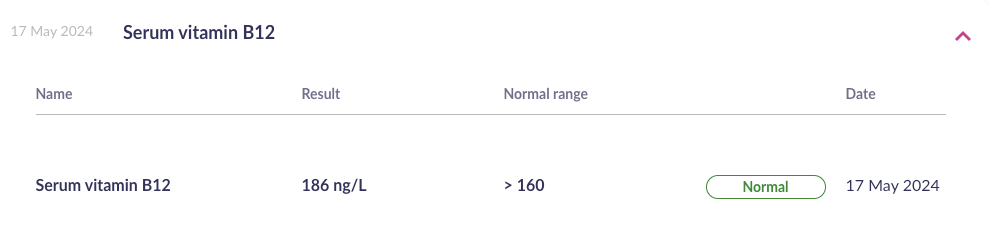
With bilateral neuro symptoms in his arms, he is 100% getting a trial of B12 in the future.
IMO it is very likely that he has un-diagnosed low grade inflammatory bowel disease, affecting his digestion/absorption, and potentially autoimmune gastritis aka pernicious anaemia.
After all that, I sent him to a rheumatologist (he has BUPA), as I couldn’t believe a rhematologist would not connect the dots and see frankly obvious auto-immue issue in process occurring.
Well, turns out I was wrong, she was adament he has costochondritis, of mechanical origin.
Sure, he has a high CRP, but probably best just to repeat it and see.
Another MRI is being planned, will there be enough damage yet to fulfil a diagnosis in the NHS?
Either way I am going to do my best to get his nutrition up and his immune system down.
A handful of supplements and a diet trial based on our ancestral heritage, and he could be in remission.
When I lecture and talk to practitioners, the most common comment I hear about why they might not want to learn any more about nutrition is “I refer out for nutrition”.
On the surface this isn’t a bad idea, but it hides a terrible lie that will hurt your patients.
Unless you knew more about biochemistry and nutrition, you would know they need to be referred out.
The GP and NHS have said they are all fine, so why would you refer out for nutrition.
I don’t do counseling for patients, I refer out for it and EMDR etc, but I have learned enough to know when that is appropriate. If I had limited understanding of how the mind affects the body and how it might present or affect my care, I simply wouldn’t know they needed it.
This, to me, is infuriating as it is willful ignorance and patients’ health is sacrificed on the altar of your ego.
And let’s be clear, I am not practicing deep nutrition on this patient.
He will get a sack of supplements, a reset diet with no gluten, dairy, eggs, nuts, soya and some Chiro care.
I am looking forward to seeing him diagnosed correctly, and then we’ll see where his care takes him.
